On December 3, 2020, the Department of Health and Human Services (HHS) offered grants to support broader use of telehealth services including in Medicare, private insurance, and through other federally funded providers – all in response to COVID.
1. Permanent Medicare changes include:
Federally Qualified Health Centers (FQHCs) and Rural Health can serve as a distant site provider for behavioral/mental telehealth services.
Medicare patients can receive telehealth services for behavioral/mental health care in their homes.
There are no geographic restrictions for originating site for behavioral/mental telehealth services.
Behavioral/mental telehealth services can be delivered using audio-only communication platforms.
Rural hospital emergency department are accepted as an originating site.
2. Temporary Medicare changes thru December 31, 2023:
· Medicare beneficiaries in any geographic area can receive telehealth services, this was a change from pre- covid rules that only beneficiaries living in rural areas.
· Beneficiaries can remain in their homes for telehealth visits reimbursed by Medicare, rather than needing to travel to a health care facility.
· In lieu of equipment with both audio and video capability, telehealth visits can be delivered via smartphone.
· Federally qualified health centers and rural health clinics can provide telehealth services to Medicare beneficiaries, regardless of provider site, rather than being limited to originating in the area where the beneficiary is located.
Note: The Consolidated Appropriations Act, 2023 extended these flexibilities through December 31, 2024, regardless of the status of the § 319 PHE; previously these flexibilities were set to expire after 151 days after the end of the § 319 PHE.
3. Temporary flexibilities set to expire on May 11, 2023 (with the end of the Covid-19 public health emergency PHE).
· For the duration of the PHE, the HHS Office for Civil Rights (OCR) exercised enforcement discretion allowing providers to use telehealth in good faith even if their platforms or software did not follow Health Insurance Portability and Accountability Act (HIPAA) rules. However, this enforcement discretion only remains in effect until the end of the PHE.
· During the COVID-19 public health emergency (PHE), authorized providers can prescribe controlled substances via telehealth, without the need for an in-person medical evaluation. The Administration’s plan is to end the COVID-19 public health emergency on May 11, 2023
· During the public health emergency, CMS waived the “established patient” requirement and allowed practitioners to bill for remote patient monitoring (RPM) for new patients. Once the PHE ends, CMS will require that RPM services be furnished only to established patients. CMS’ statements suggests after the PHE the physician must first conduct a new patient evaluation and management service before rendering RPM to such patient.
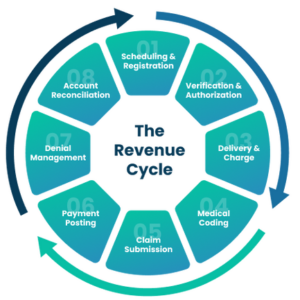
With all the changes in regulations happening with the unwinding of the Covid-19 Public Health Emergency, now more than ever it is imperative for healthcare providers to capture every dollar owed.
Titan Health specializes in supplemental staffing as well as A/R analysis and recovery, contact Titan Health today to see how we can help your hospital or organization navigate this often confusing environment and optimize your revenue cycle.